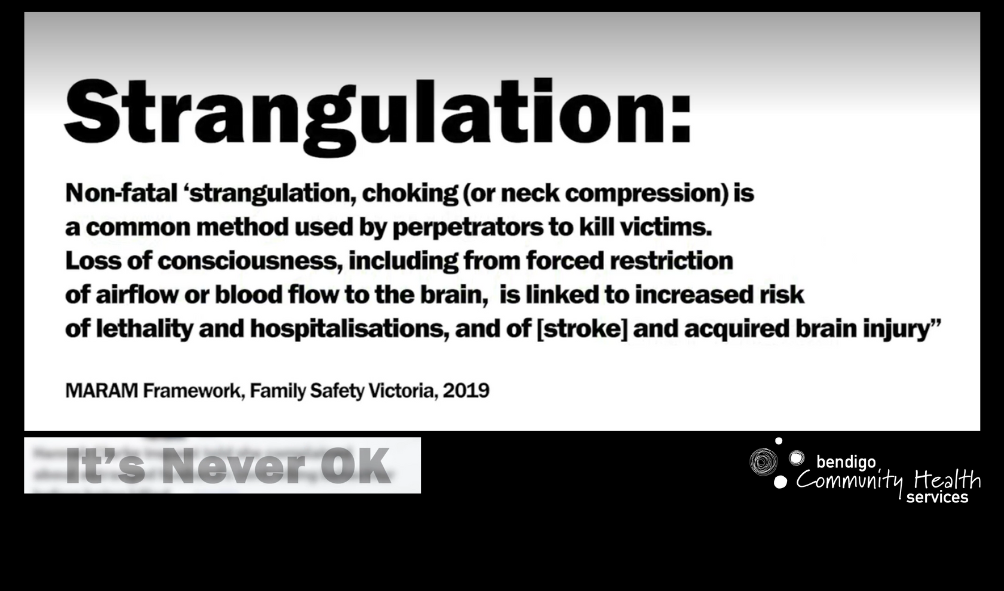
After the first episode of non-fatal strangulation, a victim survivor is seven times more likely to be killed in future events and has a one in 47 chance of experiencing a stroke later on life, particularly within the first six months.
However, for many reasons victim survivors do not or cannot disclose what happened to them, and with visible trauma to the neck only evident in 60 per cent of cases, there is still a need for improved medical responses in healthcare settings.
In partnership with Victoria Police and the Victorian Institute of Forensic Medicine, and funded by Murray Primary Health Network, BCHS produced the training video to address health responses.
A strangulation neck compression checklist and patient education discharge information sheet have also been developed.
Bendigo Community Health Services Specialist Family Violence Advisor, Meg Bagnall, says non-fatal strangulation has significant consequences for victim survivors.
“We look at the health consequences of non-fatal strangulation as one really important risk factor, for example the potential of having a stroke – but we’re also looking at the likelihood of homicide as the result of the perpetration of one episode of non-fatal strangulation,” she said.
“What we’re looking for from GPs is a referral into the family violence sector to prevent that likelihood of a fatal outcome – but we’re also looking for a medical response because the pressure applied and the trauma applied to the neck has significant health consequences.”
Victoria Police Detective Sergeant, Guy Menhennitt, of the Bendigo Family Violence Unit, says strangulation is a ‘devastating and dangerous act’ and a key indicator of lethality.
“We want medical practitioners and medical staff to be aware of the seriousness of it – and we want them to be aware that presentations to hospitals for strangulation victims is actually quite rare. Only nine per cent seek medical attention,” he said.
“So the opportunity and the privilege medical practitioners have to intervene and assist strangulation victims is so very important.
“In depth examinations and consequent imaging are vital.”
Senior Forensic Physician, Forensic Services with the Victorian Institute of Forensic Medicine, Dr Jo Ann Parkin, examines patients who have been victims of crime and is often called on to go to court to represent victims.
When someone experiences compression to the neck, Dr Parkin says it can be a harrowing experience and the victim may be under many other stresses at the time.
“It may not be their primary focus, it may be the last thing on their mind if they’re being sexually assaulted, they may be more concerned about that … they may be worried about the kids who were there in that particular incidence, so it may be something they don’t think is important,” she said.
“They might have bruises elsewhere on their body or a fracture that is distracting them, but it’s the neck compression that has underlying issues that could be really serious.
“We want to make sure we’re looking at long term problems that might be missed, and we don’t want to miss that one person that is going to have a consqeunce that is going to be life threatening.”
Detective Sergeant Menhennitt says capturing information is also critical in the justice response process.
“When we can get the accurate account, even at a medical practitioner level, it’s just as good as having it reported to police,” he said.
“By capturing that information we have it recorded officially and that can be used at any stage during the criminal justice system either now or down the track.
“To have a medical practitioner be able to analyse and find the injury, that becomes expert opinion.
“The courts rely very heavily on expert medical advice to be able to define and categorise the scope and nature of offending and that’s the single biggest factor in determining an outcome at court and therefore ultimately the safety of the vicim survivor.”
Health professionals can call VIFM for secondary consultations and further advice, and for support should they be required to give evidence in court.
The training will soon count towards continuing professional development study points for health professionals.
Strangulation Neck Compression Checklist
Strangulation Neck Compression Discharge Letter
Watch the training video below.